- Home
- Advocacy
- Latest News and Practice Data
- September 10, 2024
September 10, 2024
In this Issue:
- CAP Applauds Introduction of Physician Fee Stabilization Act in Senate
- UnitedHealthcare Launches Program to Override Prior Authorization Requirements October 1
- CAP Supports Clinical Labor Rate Updates in Medicare Fee Schedule; Urges CMS to Stop Cuts to Pathology Services
- CAP Urges CMS to Maintain Current APC level for CPT Code in Final Hospital Outpatient Regulation
- PathPAC Invests in Physician Candidates
- New CAP Webinar Series: Understanding the Impact of the FDA’s LDT Risk Classification on Your Laboratory
- Federal Agencies Work to Reassure Lab Community on Blood Culture Media Bottle Shortage
- Take Our News Quiz for September
CAP Applauds Introduction of Physician Fee Stabilization Act in Senate
On September 3, the CAP issued a press release commending the introduction of the Physician Fee Stabilization Act in the US Senate and urged Congress to enact the legislation to help prevent across-the-board Medicare cuts to physicians in future years. CAP President Donald Karcher, MD, FCAP, issued the following statement thanking sponsors Sens. John Boozman (R-AR), Peter Welch (D-VT), Thom Tillis (R-NC), Angus King (I-ME), Roger Marshall, MD (R-KS), and Jeanne Shaheen (D-NH) following the bill’s introduction:
“We are encouraged that Congress is considering long-term fixes to Medicare’s broken payment system, which has cut reimbursements for physician services year after year. Coupled with the absence of an annual update for inflation, reductions to reimbursement unrelated to the actual cost of providing care have no place in the Medicare program. The Physician Fee Stabilization Act would be a crucial step toward stabilizing the Medicare program for patients and the physicians providing care for them. The CAP appreciates the work of Sens. Boozman, Welch, Tillis, King, Marshall, and Shaheen for leading the introduction of this important bill in the Senate.”
The Physician Fee Stabilization Act would increase the budget neutrality threshold from $20 million to $53 million, followed by updated increases every 5 years to keep pace with the Medicare Economic Index. The last update to the threshold was in 1992.
In addition to the CAP, the American Medical Association and numerous other medical associations are supporting the legislation. Read the press release here.
UnitedHealthcare Launches Program to Override Prior Authorization Requirements October 1
On October 1, UnitedHealthcare is launching a national Gold Card program, which will recognize provider groups who consistently adhere to evidence-based care guidelines. Qualifying care provider groups will follow a simple notification process for eligible procedure codes rather than the prior authorization process. This advance notification will confirm eligibility and network status, but it will not require clinical information. Gold Card status will apply across UnitedHealthcare’s Commercial, Individual Exchange, Medicare Advantage and Medicaid plans.
To be eligible for gold card status, practices must show a prior authorization approval rate of 92% or higher for two consecutive years. Provider groups can now view their UnitedHealthcare Gold Card program status via the UnitedHealthcare Provider Portal
The CAP has advocated for gold card programs to reduce physician practice burdens and prevent patient care delays for many years. In a March 2023 letter, the CAP asked the Centers for Medicare & Medicaid Services (CMS) to streamline prior authorization processes in Medicare Advantage (MA) and other public health plans though gold card programs. The CAP has also successfully advocated in Arkansas for a gold card payment safeguard which ensures health plans do not deny or reduce reimbursement for pathologists who complete a service requested by an exempt gold-card provider. Wyoming recently became the second state to codify CAP’s gold card payment safeguard.
For more information on the program, including eligibility criteria and a comprehensive list of Gold Card eligible CPT codes, visit UnitedHealthcare’s national Gold Card program information page.
CAP Supports Clinical Labor Rate Updates in Medicare Fee Schedule; Urges CMS to Stop Cuts to Pathology Services
Following our efforts to protect the value of pathology services, the CAP called on the Centers for Medicare & Medicaid Services (CMS) to finalize clinical labor rate improvements in the 2025 Medicare Physician Fee Schedule and take additional steps to stop payment cuts to pathologists next year. In the CAP’s formal comments to the 2025 proposed fee schedule, the CAP also supported the appropriate valuation for apheresis services and made recommendations on changes to Medicare’s Merit-based Incentive Payment System (MIPS).
The CMS published the 2025 proposed Medicare Physician Fee Schedule and Quality Payment Program (QPP) regulation on July 10. The CAP responded to the proposed regulation with a 23-page letter on September 9 that advocated for several changes that would protect the value of pathology services and reduce regulatory burden on pathologists. In order to ensure appropriate reimbursement for all aspects of CAR-T therapy, at the request of the CMS, the CAP has provided detailed information on the practice expense costs and direct inputs associated with CAR-T, urging the Agency to carefully consider this information as it determines how bast to determine appropriate reimbursement for the CAR-T practice expense.
Appropriate Valuation of Apheresis Clinical Labor
As outlined in the 2025 Medicare Physician Fee Schedule and in support of the CAP’s efforts, the CMS proposed to update the clinical staff labor type for CPT codes 36514, 36516 and 36522 from RN/LPN to RN/OCN. This proposed change will increase the reimbursement rate for the three CPT codes in the non-facility setting. The CAP agreed with this proposal and urged the CMS to finalize the clinical labor staff type change recommended by the RUC for CPT codes 36514, 36516, and 36522.
Clinical Labor Rate Update
In general, services paid through the Medicare Physician Fee Schedule have two components: a physician work component and a technical component. The technical component represents the clinical (non-physician) labor, medical supplies, and equipment used to furnish a particular service. Clinical labor is represented as a per minute expense, with the CMS determining the rate paid for each clinical labor type. The CAP encouraged the CMS to develop a process by which stakeholders can provide updated non-physician clinical labor costs.
Advanced Alternative Payment Models (APMs)
In this rule, the CMS is proposing changes around beneficiary attribution for purposes of quality payment determinations. The proposed rule also incorporates changes made by Congress to continue the APM Incentive Payment amount of 1.88% for the 2026 payment year (performance year 2024). The CAP supports efforts to “simplify and streamline QP determinations.” However, the CAP is concerned that there is more work to be done in this area and strongly urges the CMS to, as expressed, “continue to analyze these developments and issues with the goal to provide for an equitable, rational, transparent, and meaningful methodology for QP determinations across the full range of Advanced APMs.”
CAP Offers Recommendations on MIPS
Finally, the proposed rule included a request for information on sunsetting traditional MIPS to align with the CMS’ broader goal of having Medicare beneficiaries in accountable care relationships by 2030. The CAP made multiple recommendations on evolving Medicare’s MIPS program, highlighting the importance of reducing the burden of the MIPS program and ensuring meaningful quality improvement. The CAP also expressed concern with the rapid pace of CMS’ proposed changes; constant change contributes to the burden of the MIPS program.
In the letter, the CAP also offers several suggestions regarding the future of MVP development including that specialties without a meaningful MVP would remain in traditional MIPS until MVPs evolved or until an alternative payment model was available for the clinicians, rather than forcing specialties to participate in unrelated MVPs. The CAP also supported CMS’ policies to increase the point value of certain pathology-specific measures and maintain the performance and data completeness thresholds at their current levels.
CAP Urges CMS to Maintain Current APC level for CPT Code in Final Hospital Outpatient Regulation
The CAP asked the Centers for Medicare & Medicaid Services (CMS) to reevaluate the ambulatory payment classification (APC) for clinical CAR-T services proposed 2025 Hospital Outpatient Prospective Payment System and Ambulatory Surgery Center Payment System regulations. The CAP advocates fair payment for all services pathologists provide—actively representing pathologists’ interests in every payment-related policy discussion.
Separate and Distinct Payment for CAR-T Service
In the September 9 comment letter to the CMS, the CAP argued that these clinical services occur months to weeks in advance of potential CAR-T cell infusion, and are distinct services separate from the manufacturing of the CAR-T cell product. Therefore, they should be allowed to be reported and paid separately at the time they occur. Further, each service is distinct with their own unique costs, liabilities, and clinical tasks. In its’ comments to CMS, the CAP urges the CMS to treat CAR-T services as separate and distinct physician services on the HOPPS by assigning payable status indicators and unique APC payments.
Ambulatory Payment Classification (APC) Level Changes
The CMS is proposing to move surgical pathology tissue exam by pathologist (CPT code 88309) to APC 5673 “Level 3 Pathology” from APC 5674 “Level 4 Pathology”. The CAP disagrees with this proposed change to the APC for CPT code 88309. The CAP believes the data leading to this change in APC level must be flawed. The CMS’s proposed change represents a 57% decrease in the payment amount and does not align with the much more complex set of resources required to examine these specimens. The CAP is urging CMS not to finalize this change and instead maintain the current Level 4 APC assignment.
PathPAC Invests in Physician Candidates
There are only 19 physicians serving in the 118th Congress, two of whom will retire at the end of the year. PathPAC has been dedicated to growing this number in the next Congress, recognizing the value that a medical background can bring to a lawmaker’s policy decisions.
This cycle, PathPAC has been active in connecting local CAP members with several physician candidates seeking the PAC’s support. These connections serve as an opportunity to cultivate a strong relationship and to share the top issues impacting patients and pathology. If elected, PathPAC-backed candidates have a solid foundation of knowledge to grow into pathology champions through the relationships the PAC helped develop early in the process.
Below are the profiles of two physician candidates who have received PathPAC support this election cycle. PathPAC is currently reviewing the races of two additional candidates, Maxine Dexter, MD (OR-03) and Bob Onder, MD (MO-03).
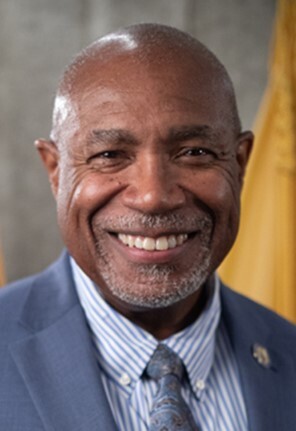
Herb Conaway, MD (NJ-03) is a former U.S. Air Force Captain, internal medicine physician, and longtime member of the New Jersey State Legislature. During his 25-year legislative career at the state level, Dr. Conaway’s medical background has informed his policy priorities, including prescription drug affordability, mental health access, and prior authorization reform. In the New Jersey Assembly, Dr. Conaway has held key leadership positions, including Deputy Speaker and Chair of the Health Committee. If elected to Congress, Dr. Conaway is motivated to put forth common sense solutions to longstanding health care challenges in his work at the federal level, just as he has done for decades in New Jersey. After winning his primary in June, Dr. Conaway is considered the frontrunner in this race, as well as one of the best opportunities for a physician to pick up an open congressional seat in November.

Kelly Morrison, MD
(MN-03) is an OB-GYN and Minnesota state senator. In her five-year career in the state legislature, Dr. Morrison has passed a record 80 bills and maintained a strong track record of bipartisanship.
Dr. Morrison understands how heavily the health care system relies on pathologists and labs, and she recently shared this sentiment when she met with a local CAP member as part of PathPAC’s candidate evaluation process.
Dr. Morrison is also the frontrunner in her race, outraising her opponent 5:1 so far. If current race ratings hold through November, Dr. Morrison will be in a strong position to join the ranks of physicians in Congress next year.

PathPAC strives to increase the political awareness of our members through political analysis, education, and helping our members build relationships with members of Congress. Learn more.
New CAP Webinar Series: Understanding the Impact of the FDA’s LDT Risk Classification on Your Laboratory

The CAP is launching a six-part webinar series to help the pathology and laboratory community understand and prepare for the Food and Drug Administration (FDA) oversight rules for laboratory-developed tests. The webinar series begins on September 18 and will focus on the FDA risk classification system.
Last April, the FDA released its regulation on the oversight of LDTs, which the CAP opposes and is advocating to stop from going into effect. Laboratories and pathologists—many having never worked with the FDA—now have questions and concerns as they face implementation of the LDT regulations first phase in May 2025.
The first webinar in our series on September 18, Noon-1 PM CT, will help laboratories understand FDA risk classification systems. We will discuss differences in classifications used by the FDA and CLIA, requirements under the FDA risk categories, and what activities the FDA includes in its general and special controls. Our experts will also discuss examples of common tests and how the FDA requirements will apply to them.
Whether you attend live or watch the on-demand recording at a time more convenient for you, register today for the first event in the series and save the dates for the upcoming webinars through July 2025.
Future webinar topics:
- November 7, 2024, Noon–1:00 PM CT, Ready Your Laboratory for the FDA’s Stage 1: Adverse Event Reporting Requirement
- January 9, 2025, Noon–1:00 PM CT, Ready Your Laboratory for the FDA’s Stage 1: Corrective Action and Removal Reporting
- March 20, 2025, Noon–1:00 PM CT, Ready Your Laboratory for the FDA’s Stage 1: Rules for Quality System Complaint Processes
- May 8, 2025, Noon–1:00 PM CT, How Enforcement Discretion Categories & Modification Rules Apply to Your LDTs
- July 10, 2025, Noon–1:00 PM CT, Navigating the FDA’s LDT Oversight Requirements During a Public Health Emergency
Federal Agencies Work to Reassure Lab Community on Blood Culture Media Bottle Shortage
Agencies within the Biden Administration have developed resources for the laboratory community to help manage disruptions in the availability of Becton Dickinson (BD) BACTEC™ blood culture media bottles.
On August 29, the Centers for Medicare & Medicaid Services (CMS) posted CLIA FAQs to about the continued shortage. The FAQs address three main stakeholder concerns regarding the blood culture shortage, including CMS awareness, the use of expired blood culture bottles, and the verification of glass blood culture bottles. Additional information can be found in the statement issued by Health and Human Services Secretary Xavier Becerra here.
On July 23, the Centers for Disease Control and Prevention issued a health advisory about the critical shortage of blood culture media bottles. The advisory followed an announcement by the Food and Drug Administration regarding the disruption in availability of BD BACTEC blood culture media bottles on July 10.
The CAP will continue to monitor the situation and will keep members informed of the latest updates and resources.
