- Home
- Advocacy
- Latest News and Practice Data
- December 19, 2023
December 19, 2023
In this Issue:
- Register for the Pathologists Leadership Summit in D.C. April 2024
- Federal IDR Process Administrative Fee Final Rule Released
- Federal IDR Surprise Billing Portal Reopened for All Dispute Types December 15
- New Health IT Final Rule Has Minimal Impact on Pathology
- PathPAC Members Meet Sen. Duckworth to Discuss Health Care Priorities
- ONC Releases New Platform to Centralize Electronic Health Data
- CDC Publishes Testing Guidance for Patients with Viral Hemorrhagic Fevers and Rocky Mountain Fever
- Take Our News Quiz for December
- Editor’s Note
Register for the Pathologists Leadership Summit in D.C. April 2024
Year after year, pathologists’ payments are being threatened to decline, workforce shortages are causing burnout, and cuts to clinical laboratory payments hang in the balance.
Advocate for pathology and plan to attend the Pathologists Leadership Summit in-person where you will gain unparalleled access to the education and training to make an impact on Capitol Hill and protect the future of our specialty.
The Pathologists Leadership Summit takes place, in-person only, April 13-16 in Washington, DC. Mark your calendars and register today!

Federal IDR Process Administrative Fee Final Rule Released
On December 18, the Department of Health and Human Services (HHS), jointly with the Departments of Labor and the Treasury, issued a final rule outlining the fees for the Federal Independent Dispute Resolution (IDR) process under the No Surprises Act. The CAP argued that especially with the administrative fee, as it is non-refundable, ANY increase in the fee amount imposes added burdens and potentially a complete barrier for physicians in accessing the federal IDR process. The CAP believes it is vital that any fee requirements take into consideration low-dollar claims and ensure an even and fair playing field for all IDR parties.
Acknowledging these concerns, this rule finalizes an administrative fee amount of $115 per party for disputes initiated on or after the effective date of this rule, down from the proposed $150. It finalizes an IDR entity fee range of $200-$840 for single determinations and $268-$1,173 for batched determinations for disputes initiated on or after the effective date of the rule. However, the Departments are in the process of additional rulemaking around the IDR process and its fees, including a reduced administrative fee for low dollar claims as requested by the CAP. The CAP will submit comments on this latest rulemaking by the deadline of January 2, 2024.
Federal IDR Surprise Billing Portal Reopened for All Dispute Types December 15
On December 15, the federal government reopened the independent dispute resolution (IDR) process and began accepting all dispute types after being shut down since August. The Centers for Medicare and Medicaid Services closed the portal as a result of the Texas Medical Association v. United States Department of Health and Human Services case where the judge ruled in favor of physicians on August 3.
The portal was later reopened for single disputes but not for batched disputes. The CMS’ latest action reopened the federal IDR portal to process all dispute types, including previously initiated batched disputes, new batched disputes, and new single disputes involving air ambulance services.
According to the CMS website, parties for whom the IDR initiation deadline under applicable regulations fell on any date between August 3, 2023, and December 15, 2023, will have until January 16, 2024, to initiate a new batched dispute.
Parties for whom the IDR initiation deadline falls between December 16, 2023, and January 15, 2024, will also have until January 16, 2024, to initiate a batched dispute. Parties whose initiation deadline falls on January 16, 2024, or after will have the usual 4 business days after the end of the Open Negotiation Period, or if the dispute is subject to the 90-calendar-day suspension period following a payment determination, the usual 30 business day period, to initiate a batched or air ambulance dispute in the federal IDR portal.
In addition, the deadline to submit fees and offers will remain 10 business days after certified IDR entities are selected. Read more.
New Health IT Final Rule Has Minimal Impact on Pathology
On December 13, the Office of the National Coordinator for Health Information Technology (ONC) released the Health Data, Technology, and Interoperability: Certification Program Updates, Algorithm Transparency, and Information Sharing (HTI-1) Final Rule, which updates the ONC Health IT Certification Program. The purpose of this final rule was to advance interoperability, improve transparency, and support the access, exchange, and use of electronic health information.
The CAP’s priority issues in the HTI-1 proposed rule were:
- Laboratory Data Interoperability Request for Information:
In a June 20 comment letter, the CAP stated that because the laboratory ecosystem is uniquely broad and complex, certification of Laboratory Information Systems (LIS) is not currently feasible. The ONC did not implement LIS certification in this final rule. - Artificial Intelligence:
The ONC finalized transparency requirements for the artificial intelligence (AI) and other predictive algorithms that are part of certified health IT. This provision is effective December 31, 2024. The CAP supported this provision. - USCDI v3:
The CAP supported the transition from United States Core Data for Interoperability (USCDI) Version 1 to USCDI Version 3. In the Final Rule, the ONC set USCDI Version 3 to replace USCDI Version 1 as the baseline USCDI standard for ONC Certification as of January 1, 2026. - Patient Requested Restrictions Certification Criterion:
The CAP had supported the “Patient Requested Restrictions Certification Criterion” as written in the HTI-1 proposed rule. In the final rule, the ONC decided not to finalize most of their proposals for patient requested restrictions at this time. - Information Blocking: The CAP supported the Information Blocking Provisions but reiterated the need for additional work on Information Blocking rules as it relates to reducing potential patient harm and improving care coordination by allowing some limited blanket delays for specific kinds of tests. In the final rule, the ONC refined its definition of terms such as “offer health IT” and the ONC also revised two exceptions (the Infeasibility and Manner exceptions) and created a new exception to the Information Blocking Rule.
Because the ONC decided to defer any action on laboratory information system (LIS) certification to future rulemaking, the final rule will have minimal direct impact on pathology.
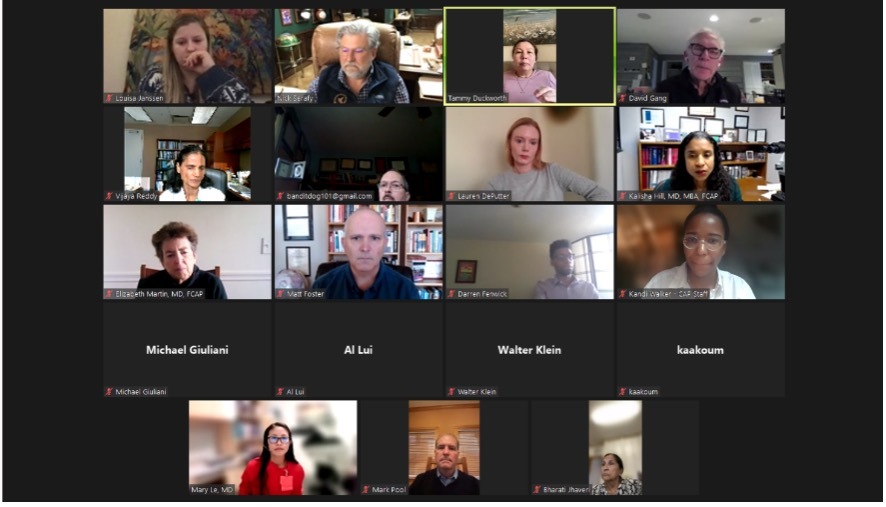
PathPAC Members Meet Sen. Duckworth to Discuss Health Care Priorities
On December 11, a group of 20 PathPAC members met virtually with Sen. Tammy Duckworth (D-IL) for a “fireside chat” as Congress wraps up the year. PathPAC supports and represents the interests of pathologists on Capitol Hill through political and financial means. PathPAC works to increase the political awareness of our members through political analysis, education, and helping our members build relationships with members of Congress.
Sen. Duckworth highlighted some of her health priorities which include:
- Physician workforce development
- Increasing diversity in health care
- Addressing the country’s high maternal mortality rate
- Filling rural health care gaps
- Concern that insurance companies will want to use artificial intelligence (AI) to eliminate doctors. She feels Congress should establish appropriate standards and guardrails for its use.
The Senator told the group that the issue of physician Medicare cuts is on the priority list for Democrats and Republicans. In her opinion, Medicare reform is less likely to happen because Democrats and Republicans have different views on what reform looks like. She said, “Congress will still talk about it, but we will likely see more stop gap measures.”
PathPAC provides the best opportunity to elect lawmakers to Congress that will make fair and reasonable policies towards pathology. Contributing to PathPAC also shows support for the advocacy efforts of CAP members and staff. Learn more and get involved with PathPAC.
ONC Releases New Platform to Centralize Electronic Health Data
The Office of the National Coordinator for Health Information Technology (ONC) has released a new USCDI+ platform. The USCDI+ platform enables users to see in and across a standardized set of health datasets for comparison and analysis for a broader sharing of electronic health information to support patient care. The platform also includes the ability to filter and export data elements by information within the datasets, as well as advanced logic to help reduce duplicate data element submissions, and more.
The USCDI standard, which the ONC adopted in the 21st Century Cures Act defines how health care data must be formatted to be exchanged electronically nationwide. The CAP’s positioning on the USCDI is that the ONC should align the USCDI with the test reporting requirements in CLIA, and that the ONC should seek to achieve its goal with USCDI without overburdening pathologists and laboratories.
The ONC is also accepting data element submissions and comments for two USCDI+ Public Health use cases: Case Reporting and Laboratory Data Exchange. The comment period ends on March 4, 2024, with updated datasets to be released in late Spring.
CDC Publishes Testing Guidance for Patients with Viral Hemorrhagic Fevers and Rocky Mountain Fever
The Centers for Disease Control and Prevention (CDC) recommended that clinical laboratories review the testing guidance for viral hemorrhagic fevers (VHF) - a group of diseases caused by several distinct families of viruses. The term “viral hemorrhagic fever” refers to a condition that affects multiple organ systems of the body, damages the overall cardiovascular system, and reduces the body’s ability to function on its own.
VHFs are caused by infection with any of the following viruses: ebolaviruses, marburgviruses, Crimean-Congo hemorrhagic fever virus, arenaviruses (Lassa, Lugo, and South American hemorrhagic fever viruses), and Nipah virus.
While the risk of VHFs being brought into the US by travelers is very low, the CDC recommends that clinical laboratories review the testing guidance:
- Guidance for US Hospitals and Clinical Laboratories on Performing Routine Diagnostic Testing for Patients with Suspected Ebola Disease
- Guidance for Collection, Transport, and Submission of Specimens for Ebolavirus Testing
If testing determines a patient has a VHF, clinical teams should coordinate with public health officials and the CDC to ensure appropriate precautions are taken to help prevent the potential spread and coordinate care.
The CDC also issued a Health Alert Network (HAN) message about an outbreak of Rocky Mountain spotted fever (RMSF) among people in the United States with recent travel to or from the city of Tecate, state of Baja California, Mexico. If RMSF is suspected, whole blood and serum samples obtained from acutely ill people should be evaluated for Rickettsia by molecular and serologic testing methods available at commercial laboratories, state public health laboratories, or CDC.
Take Our News Quiz for December
Are you up to speed on CAP advocacy news? Take our new monthly news quiz and see how many you can get right and share your results on social media.
Editor’s Note
Due to the Christmas and New Year’s holiday, the next edition of Advocacy Update will be January 9. If important news breaks, the CAP will send a special edition of the newsletter or post information on our Twitter account @CAPDCAdvocacy.